Despite being an essential part of the insurance life cycle, claims is often still viewed as a cost center. While the emergence of new catastrophes has indeed raised the amount insurers are paying in claims — the first half of 2023 showed insurers spending 104.3 cents on expenses and claims for every 100 cents they gained in premium — there are opportunities to modernize the insurance claims process and create value for the business.
Claims modernization is a major undertaking, and even insurers who have updated their systems may not have had the chance to modernize the manual processes that accompany those systems. Crafting a truly modern insurance claims management strategy requires organizations to simplify processes where possible with modern technology, improve their customer and adjuster experiences, and plan proactively for increases in catastrophe and fraud.
This blog post explores three trends shaping the insurance claims world in 2024 and beyond and offers suggestions to insurance IT leaders for how to successfully build a modern claims experience that will satisfy customers and lead to future success.
3 Major Trends in Insurance Claims
The introduction of ChatGPT in 2023 created a monumental shift within almost every industry, and insurance is no different. While insurance has already seen more cloud adoption and a stronger pull toward modern data and analytics practices, combining these with generative AI models provides opportunities for increased efficiency and accuracy across the insurance value chain.
This shift can already be seen within claims, where generative AI is being used to help claims adjusters generate reports, communicate with customers, and create marketing materials. Those aren’t the only places where generative AI and other modern technologies are being used to create a more empathetic claims process and ultimately help grow claims revenue.
Here are three areas where insurers are working to modernize their claims process:
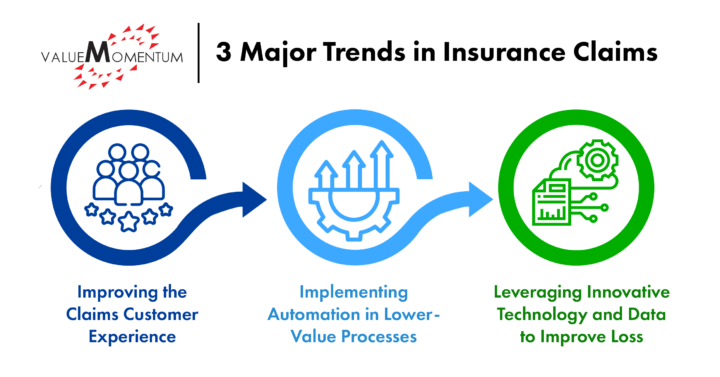
- Improving the Claims Customer Experience
An experience bolstered by cloud adoption, advanced data and analytics, and generative AI can help keep up with demands for real-time, seamless, and omnichannel interactions from newer generations of customers. As cloud adoption accelerates, insurers gain the ability to be more flexible and agile. They no longer have to work through legacy systems in order to deliver quickly. In addition, the cloud can help improve insurers’ access to tools like advanced data and analytics and generative AI.
Data and analytics technology, along with generative AI and other large language models, can take on the heavy lifting to sort documents, extract relevant passages and summarize large passages, identify red flags, and more. Generative AI can also be used to help detect potential fraud by analyzing anomalies, reviewing historical claims data, and identifying connections between those involved in the claim. Amica Mutual, for example, developed and trained a predictive model to replace its existing manual review process. It’s expected to reduce the claims assignment time while increasing the amount of desk-adjusted claims, providing a better experience for customers and adjusters alike.
- Implementing Automation in Lower-Value Processes
McKinsey & Company found that by 2030, over 50 percent of current claims activities might be automated. Today’s advanced insurers use automation to handle routine claims, which account for almost 60 percent of global claims volume, so they can focus human attention on claims that are more sensitive, aremore complex, and require greater care and empathy.
Robotic process automation (RPA) can be used to take on tasks that are routine and repeatable, such as data entry, manual reviews, and calculations. Such lower-value processes can take up a lot of time in an employee’s day or even week. By taking these tasks off their plate, claims teams can spend more time focusing on customers while speeding up the claims process and making it more accurate and efficient. As insurers settle claims faster and build stronger relationships with their customers, they’ll gain opportunities for more revenue growth.
- Leveraging Innovative Technology and Data to Improve Loss
Catastrophe losses have increased substantially in the past few years. Combined with the cost of inflation and higher reinsurance costs, the U.S. combined ratio has surpassed 100 for five out of the last six years. But claims leakage also contributes to such losses. Claims leakage can be resolved, however, with the same process automation and optimization mentioned above. Because while losses have increased, so have claims handling processes, which means that companies have not gained efficiency while handling more claims.
As companies leverage new technologies, they’re able to see a shift in claims leakage even with a higher combined ratio than in previous decades. For example, a Fortune 500 insurer recently rolled out an AI-model-driven system built on AWS to help combat, among other challenges, problems with subsidizing policyholders filing preventable claims. The integration of AI and aerial imagery resulted in $3.5M saved annually even with reduced instances of claim denials.
How to Drive Success With Claims Modernization
- Balance Human and Digital Interactions

While a customer may have no problem filling out a form online to receive their payment, and they may be more comfortable with a quick direct deposit over a mailed check, they might not be comfortable speaking to a chatbot about recently losing their home.
As companies update their customer experience with automation and other modern tools, they may also inadvertently make the customer experience more fraught. Filing a claim can be a very emotional time, so speed, transparency, and empathy are critical to the claims experience. And while automation can play a strong role in speed and transparency, it cannot replace receiving empathy from another human.
- Start Small Before Going Big With Automation
 When implementing new tools like automation and generative AI, start small to both determine what part of the claims process will benefit most and gain companywide buy-in. Insurers can start by thinking about processes where automation can easily be incorporated, such as scanning documents and providing summaries.
When implementing new tools like automation and generative AI, start small to both determine what part of the claims process will benefit most and gain companywide buy-in. Insurers can start by thinking about processes where automation can easily be incorporated, such as scanning documents and providing summaries.
Even this one small change can reduce the amount of time team members focus on manual processes when they could be connecting with customers. Once the organization sees how effective the change is, insurers can then use the learnings from the test project to focus on a longer-term transformation.
- Harness Agile Change Management for Adoption Success
 One of the biggest reasons companies don’t digitalize or adopt new processes is a resistance to change. Even when an organization has already executed a transformation, many team members may not adopt the technology, leading to excessive spending on multiple platforms as team members struggle to transition and leaving customers waiting as manual processes take longer.
One of the biggest reasons companies don’t digitalize or adopt new processes is a resistance to change. Even when an organization has already executed a transformation, many team members may not adopt the technology, leading to excessive spending on multiple platforms as team members struggle to transition and leaving customers waiting as manual processes take longer.
Organizations that are finding their teams still using legacy systems or processes may need to review their company culture and change management processes to help their teams become amenable to change. To help, insurers should establish an Agile change management process that uses regular training sessions, sends frequent communications, and includes end users in decision-making processes. This will help build buy-in as the claims journey evolves to a more modern practice.
Reimagining the Insurance Claims Journey
The claims journey is being reimagined from beginning to end, encompassing people, processes, and technology. When done holistically, finding the right balance of decreasing manual work with automation, reducing fraud with innovative tools, and building loyalty with customers through an empathetic claims process will help improve revenue as a result of claims, not in spite of it.
To learn more about how insurers are modernizing their claims processes to improve efficiency, reduce losses, and improve customer experience, dive into our case study, “Motor Insurer Automates Claims Settlement Process.”
